cervical radiculopathy physical therapy protocol pdf
Cervical Radiculopathy Physical Therapy Protocol
This guide provides a comprehensive overview of a physical therapy protocol for cervical radiculopathy, a condition characterized by nerve root compression in the neck. It outlines the phases of treatment, recommended exercises, and home care strategies to help patients regain function and reduce pain. The protocol is based on current research and evidence-based practices, and aims to provide a structured approach to physical therapy for individuals with cervical radiculopathy.
Introduction
Cervical radiculopathy, often referred to as a pinched nerve in the neck, is a common condition that affects millions of people worldwide. It occurs when a nerve root in the cervical spine, the area of the spine in the neck, becomes compressed or irritated. This compression can result from various factors, including herniated discs, bone spurs, and spinal stenosis. The condition can lead to a range of symptoms, including neck pain, radiating arm pain, numbness, tingling, and weakness.
Physical therapy plays a crucial role in the management of cervical radiculopathy. A well-designed physical therapy protocol can help reduce pain, improve mobility, restore function, and prevent future episodes. This protocol outlines a comprehensive approach to physical therapy for cervical radiculopathy, encompassing various phases of treatment, specific exercises, and home care strategies.
Causes and Symptoms
Cervical radiculopathy arises from compression or irritation of the nerve roots that exit the spinal cord in the neck. Several factors can contribute to this compression, including⁚
- Herniated discs⁚ When the soft, jelly-like center of an intervertebral disc protrudes or ruptures, it can press on the nearby nerve root.
- Bone spurs⁚ Osteophytes, or bone spurs, can develop along the vertebrae and narrow the space for nerve roots, leading to compression.
- Spinal stenosis⁚ This condition involves narrowing of the spinal canal, which can put pressure on the nerve roots.
- Degenerative changes⁚ Aging and wear and tear on the cervical spine can lead to changes in the discs and joints, contributing to nerve root compression.
The symptoms of cervical radiculopathy vary depending on the specific nerve root affected and the severity of compression. Common symptoms include⁚
- Neck pain, often radiating to the shoulder, arm, or hand.
- Numbness, tingling, or weakness in the arm or hand.
- Decreased sensation in the affected area.
- Muscle weakness or difficulty with fine motor skills.
Conservative Treatment
The primary goal of conservative treatment for cervical radiculopathy is to reduce pain, inflammation, and nerve compression, thereby improving function and quality of life. A multidisciplinary approach is often employed, involving a combination of treatments tailored to the individual patient’s needs. Common conservative interventions include⁚
- Medications⁚ Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and sometimes opioids are prescribed to manage pain and inflammation.
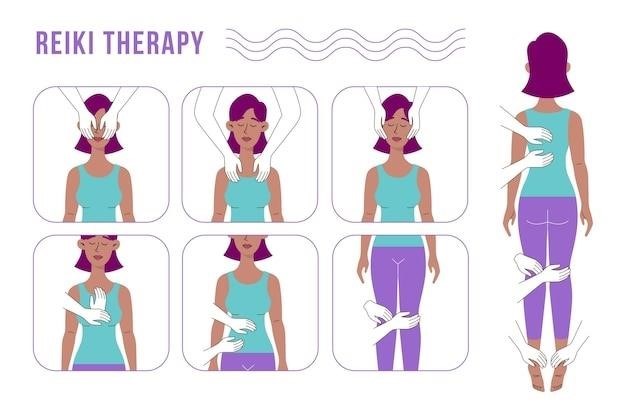
- Physical therapy⁚ A physical therapist can guide patients through a personalized exercise program designed to strengthen muscles, improve range of motion, and promote proper posture. Manual therapy techniques, such as joint mobilization and soft tissue mobilization, may also be employed to address musculoskeletal restrictions.
- Cervical traction⁚ This technique involves gently stretching the neck to reduce pressure on the nerve roots. It can be performed manually or with a specialized traction device.
- Injections⁚ In some cases, corticosteroid injections may be administered into the affected area to reduce inflammation and pain.
- Lifestyle modifications⁚ Adjusting daily activities to avoid aggravating factors, such as prolonged sitting, repetitive movements, and heavy lifting, can help manage symptoms.
In many cases, conservative treatment can effectively alleviate cervical radiculopathy symptoms and restore function. However, if symptoms persist despite conservative measures or if neurological deficits worsen, surgical intervention may be considered.
Physical Therapy Protocol
A structured physical therapy protocol for cervical radiculopathy typically involves three phases, each with specific goals and exercises designed to progressively restore function and reduce pain. This phased approach allows for a gradual increase in activity levels as the patient’s condition improves. The phases include⁚
- Phase 1⁚ Acute Phase (Week 1-2)⁚ Focuses on pain management and inflammation reduction. Exercises may include gentle range of motion exercises, postural correction techniques, and modalities like ice or heat therapy. The goal is to reduce pain and inflammation to allow for more advanced exercises in subsequent phases.
- Phase 2⁚ Subacute Phase (Week 3-6)⁚ Emphasizes increasing mobility and strength while maintaining pain control. Exercises may progress to include strengthening exercises for the neck and shoulder muscles, as well as proprioceptive exercises to improve balance and coordination.
- Phase 3⁚ Chronic Phase (Week 7+)⁚ Focuses on restoring functional capacity and preventing recurrence. Exercises may include more advanced strengthening and endurance exercises, as well as activities that mimic daily tasks to help patients return to their desired activities.
The specific exercises and progression through the phases will be tailored to the individual patient’s needs and response to treatment. Regular communication with the physical therapist is essential to ensure the program is adjusted as needed.
Phase 1⁚ Acute Phase (Week 1-2)
The primary focus of the acute phase is to reduce pain and inflammation, creating a foundation for further rehabilitation. This phase typically lasts for the first two weeks of treatment. Here are some key elements of the acute phase⁚
- Pain Management⁚ The physical therapist will work with the patient to identify effective pain management strategies. This may involve modalities like ice or heat therapy, manual therapy techniques to reduce muscle tension, and patient education on proper posture and body mechanics. The goal is to decrease pain to a manageable level to allow for movement and exercise.
- Rest and Protection⁚ During this phase, activities that exacerbate symptoms should be avoided. The therapist may recommend limiting certain movements and activities that increase pain. The patient is encouraged to participate in gentle activities that do not cause pain.
- Gentle Range of Motion Exercises⁚ These exercises help to maintain joint mobility and prevent stiffness. The therapist will guide the patient through gentle head and neck movements, focusing on controlled and pain-free motion. Exercises should be performed within the patient’s pain tolerance.
- Postural Education⁚ Proper posture is crucial in managing cervical radiculopathy. The therapist will educate the patient on maintaining a neutral spine, avoiding prolonged positions that strain the neck, and practicing proper sitting and standing postures.
The therapist will closely monitor the patient’s progress and adjust the treatment plan as needed during this phase.
Phase 2⁚ Subacute Phase (Week 3-6)
As pain levels subside and inflammation decreases, the focus shifts to increasing mobility, restoring strength, and improving function. This subacute phase typically spans weeks 3 through 6 of treatment. Here are some key elements of this phase⁚
- Increased Range of Motion Exercises⁚ The physical therapist will gradually increase the intensity and complexity of range of motion exercises. These exercises will involve more controlled movements and may incorporate stretches to address tightness in the neck and shoulder muscles.
- Strengthening Exercises⁚ The therapist will introduce exercises to strengthen the muscles that support the neck and shoulders. These exercises may include isometric holds, resistance bands, and light weights. The goal is to improve muscle strength and endurance, providing better support for the neck.
- Proprioceptive Training⁚ Proprioceptive exercises enhance body awareness and coordination. These exercises may involve balance activities and controlled movements that challenge the patient’s ability to sense their body position in space.
- Functional Exercises⁚ As strength and flexibility improve, the therapist will begin incorporating functional exercises that mimic everyday activities. These exercises may include tasks like reaching overhead, turning the head, and lifting objects. The goal is to help the patient safely return to their desired activities.
Throughout this phase, the therapist will continue to monitor the patient’s progress, adjusting the exercises and intensity as needed to ensure safety and effectiveness.
Phase 3⁚ Chronic Phase (Week 7+)
The chronic phase of physical therapy for cervical radiculopathy focuses on maintaining the gains achieved in the earlier phases and maximizing functional independence. This phase typically begins around week 7 and continues as needed, depending on the patient’s progress and individual goals.
- Advanced Strengthening Exercises⁚ Exercises will become more challenging, using heavier weights or resistance bands to further improve muscle strength and endurance. The focus shifts to building strength in specific muscle groups that are essential for everyday tasks and activities.
- Functional Training⁚ This phase emphasizes activities that closely mimic the demands of the patient’s daily life. The therapist may incorporate exercises that involve lifting, carrying, reaching, and rotating the head, simulating real-world movements.
- Ergonomic Education⁚ The therapist will provide guidance on proper posture, body mechanics, and workplace ergonomics to help prevent future episodes of cervical radiculopathy. This may involve making adjustments to the patient’s work environment, providing tips for safe lifting, and recommending exercises to maintain good posture.
- Home Exercise Program⁚ The therapist will develop a personalized home exercise program that the patient can continue independently. This program should include exercises that target specific muscle groups, improve flexibility, and maintain good posture. The therapist will provide detailed instructions and demonstrate the correct form for each exercise.
During this phase, the therapist will continue to monitor the patient’s progress and provide support as they transition back to their desired activities and an active lifestyle.
Exercises
Exercises play a crucial role in the rehabilitation process for cervical radiculopathy. They help to strengthen muscles, improve flexibility, restore range of motion, and reduce pain. The exercises recommended will vary depending on the individual’s specific condition, pain levels, and stage of recovery. A physical therapist will guide patients through a tailored exercise program, ensuring proper form and progression. It’s important to note that all exercises should be performed with caution and within pain limits. If any exercise causes significant pain, stop immediately and consult with the therapist.
The exercises may include stretches, strengthening exercises, and proprioceptive exercises designed to improve balance and coordination. Examples of common exercises include⁚
- Neck Flexion and Extension⁚ Gently tilting the head forward and backward, keeping the shoulders relaxed.
- Neck Rotation⁚ Turning the head slowly from side to side, keeping the chin level.
- Scapular Retraction⁚ Pulling the shoulder blades back and together, as if trying to squeeze a pencil between them.
- Isometric Neck Holds⁚ Holding the head in a specific position for a few seconds, engaging the neck muscles.
- Shoulder Shrugs⁚ Lifting the shoulders up toward the ears, then slowly lowering them back down.
It’s important to remember that these are just a few examples, and the specific exercises will be tailored to the individual’s needs.
Recommended Exercises
The goal of recommended exercises is to gradually increase range of motion, strengthen muscles, improve posture, and reduce pain. They are typically introduced progressively, starting with gentle movements and gradually increasing intensity and complexity as the patient’s condition improves. These exercises should be performed within a pain-free range, and any discomfort should be reported to the physical therapist.
Here are some examples of commonly recommended exercises for cervical radiculopathy⁚
- Chin Tucks⁚ Gently tucking the chin towards the chest, holding for a few seconds, and repeating.
- Scapular Retraction⁚ Pulling the shoulder blades back and together, as if trying to squeeze a pencil between them, holding for a few seconds, and repeating.
- Neck Rotations⁚ Slowly rotating the head from side to side, keeping the chin level, and repeating.
- Shoulder Shrugs⁚ Lifting the shoulders up towards the ears, then slowly lowering them back down, and repeating.
- Isometric Neck Holds⁚ Holding the head in a specific position for a few seconds, engaging the neck muscles, and repeating.
These exercises are designed to improve neck flexibility, strengthen neck and shoulder muscles, and improve posture. It’s important to consult with a physical therapist for personalized recommendations and proper technique.
Exercises to Avoid
While exercise is crucial for recovery from cervical radiculopathy, certain movements can exacerbate symptoms and potentially worsen the condition. It’s essential to avoid activities that cause pain or increase discomfort, as these may indicate further nerve irritation or compression. It’s important to remember that everyone’s experience with cervical radiculopathy is unique, and the specific exercises to avoid will vary depending on the individual’s specific condition and symptoms.
Here are some common exercises that should be avoided in the acute phase of cervical radiculopathy⁚
- High-impact activities⁚ Activities that involve sudden jolts, forceful movements, or repetitive strain on the neck, such as running, jumping, or contact sports.
- Heavy lifting⁚ Lifting objects that put significant stress on the neck and shoulders, which can increase pressure on the nerve roots.
- Prolonged sitting or standing⁚ Maintaining the same position for extended periods, which can contribute to muscle strain and stiffness.
- Rapid head movements⁚ Jerking or quickly turning the head, which can aggravate the nerve root irritation.
- Exercises that cause pain or numbness⁚ Any movement that reproduces or worsens the symptoms of cervical radiculopathy, such as pain radiating down the arm or tingling in the fingers.
If you experience any pain or worsening of symptoms, it’s crucial to stop the exercise immediately and consult with your physical therapist.